Online classes, masks, and needle anxiety: the obstacles and solutions for the COVID-college student experience
I am envious of the Tufts students who will have their school concerts, sports games, in-person meetings and classes, and graduation. Frankly, I felt like I wasn’t a student long before I ever got my diploma because of the pandemic. #HacktheVax is about more than the tailgating and dining hall sundaes I missed out on, or even that current students may as well. These campaigns can connect such a key population with easy and free resources to overcome needle anxiety.

Jody Thomas, PhD
Tweens & Teens (12+) Covid-19 Needle Pokes Procedural Pain English Pain Management
Share this:
In March of 2020 I got an email with the subject, “COVID-19 Update: significant and immediate changes to Tufts’ operations.” Moments later, everyone was on their phones with loved ones, crying and nervously laughing. Friends and I decided we should say goodbye to seniors instead of studying for upcoming exams. In the first hours of the pandemic on campus, we could not imagine the impact the virus would have; disproportionately on Black, Latinx, and POC communities; and on our college careers. A year later, we were used to wearing layers and bringing sleeping bags to dinners on friends’ porches in the Boston winter in order to safely socialize. Having an indoor meal between vaccinated friends felt as foreign as our first Zoom classes, but more exciting.
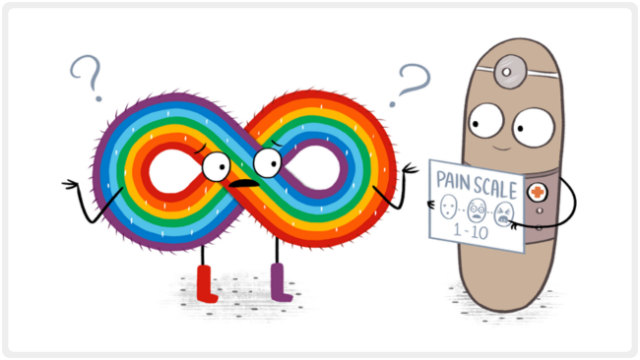
Many of my friends were itching to “get back to normal” before college ended. To get vaccinated quickly some lied about comorbidities or traveled out of state. Naturally, I felt doubtful to hear that 25% of adolescents, 50% of adults, and somewhere in-between of college students are anxious enough about needles and pain to influence their healthcare decisions and immunizations. Then again, when was the last time I, or anyone I know, talked about needle fear? Once we went to college we were adults, perfect and without any anxieties (sarcasm implied)!
I have a few vivid memories of getting vaccines as a kid. One day I asked my mom if I was going to get any shots from the doctor, to which she replied no. I remember crying when the nurses came in and held down my legs as I got two shots in each. I was privileged enough to have a physician for a dad who brought our shots home after that. A shot from your dad with cartoons playing in the background was massively easier than alone in a cold doctor’s office. In thinking about that 25% number, it seems obvious that essentially nobody got the vaccination experience I did. If I had many more experiences like that day my mom said no, I would not be lining up for a vaccine now, much less talking about that anxiety with peers.
The evidence is clear, though honestly surprising at first, that needle anxiety is an underrecognized problem that affects individuals and public health, especially coming out of the pandemic. Dealing with needles and needle anxiety is a skillset that is easy, free, and can be learned to solve that problem. College is where many develop their beliefs and habits for better or worse. Getting college students vaccinated is about much more than “returning to normal,” #HacktheVax can help students feel comfortable getting vaccinated, create an environment where there is no shame in talking about pain, and cultivate a generation (and they can cultivate the next) that can express their concerns to providers.
I am envious of the Tufts students who will have their school concerts, sports games, in-person meetings and classes, and graduation. Frankly, I felt like I wasn’t a student long before I ever got my diploma because of the pandemic. #HacktheVax is about more than the tailgating and dining hall sundaes I missed out on, or even that current students may as well. These campaigns can connect such a key population with easy and free resources to overcome needle anxiety. Starting a dialogue about and destigmatizing needle anxiety, teaching basic pain management skills, and empowering future leaders to carry that conversation is critical to public health far beyond college, and beyond COVID.
You May Also Be Interested In

Blog Post
Helping Kids Cope? Yeah, It’s Kinda Our Thing
Child Life Specialists are the undercover superheroes of pediatric healthcare—and when they team up with the Meg Foundation? Let’s just say pain, fear, and anxiety don’t stand a chance.

Blog Post
Chronic Pain Is On The Rise—Here’s What You Can Do About It Now
Earlier this week, The Washington Post featured a startling stat in their Big Number series: nearly 1 in 4 adults in the U.S. experienced chronic pain last year. And that is up from 20.4% in 2019! Let that sink in.

Blog Post
Nine reasons why pain management is a big deal
Even though we all live with it, we still get asked—usually by someone who isn’t currently in pain—‘Is it really that big a deal?’ As a pain nonprofit, we can say with complete confidence: Heck yes, it is!
Blog Post
How Pain Affects Autistic People and What We Can do to Help
Danielle Hall from the Autism Society sheds light on the unique ways autistic individuals experience and communicate pain. Her insights help us understand why recognizing their discomfort can be challenging—and how we can better support them. Let’s dive into her guidance on providing more compassionate care.

Podcast
Jewish Orthodox Women's Medical Association Podcast: Hurt, Not Harm, Preventing Pain and Trauma with Dr. Jody
Join Dr. Jody Thomas as she dives into the future of pain management, where psychology, proactive strategies, and virtual reality are transforming how we support kids through tough moments. From busting myths to sharing real patient success stories, this episode is packed with insights for anyone looking to prevent pain and trauma.

Sarah Wiener holds a BA in Political Science and Philosophy from Tufts University where she worked with administrators as Student Body President as the school responded to the COVID-19 pandemic. She is passionate about equitable accessibility to public health resources, like the work the Meg Foundation is doing.

About the Author
Dr. Jody Thomas is a licensed clinical psychologist, and specialist in pediatric medical illness and trauma. A well-known expert in pediatric pain who teaches internationally on the subject, she is also a founder and the former Clinical Director of the Packard Pediatric Pain Rehabilitation Center at Stanford, and a former Assistant Professor at the Stanford University School of Medicine. Though she now lives in Denver, CO, she still serves as Adjunct Faculty for Stanford, providing supervision and teaching. As a consultant for the Lucile Packard Children’s Hospital at Stanford, she directs projects on the integration and innovation of pain management using tech-based intervention. Her passion for bringing together the power of medical science, technology and design to transform the way we think about kids and pain led her to her current focus but it’s her role as a mom of two that solidified her path in creating the Meg Foundation.
