How Pain Affects Autistic People and What We Can do to Help
Danielle Hall from the Autism Society sheds light on the unique ways autistic individuals experience and communicate pain. Her insights help us understand why recognizing their discomfort can be challenging—and how we can better support them.
Danielle Hall
Kids (3-11) Tweens & Teens (12+) Provider Acute Pain Chronic Pain Procedural Pain English
Share this:
Everyone experiences pain at some point in their life, but did you know that people feel pain differently? Some people are highly sensitive to even minor injuries, while others may barely notice severe pain. This is called your “pain threshold,” and it varies from person to person based on a lot of different factors, including genetics, culture, gender, past pain experiences, trauma, mood, and overall health.
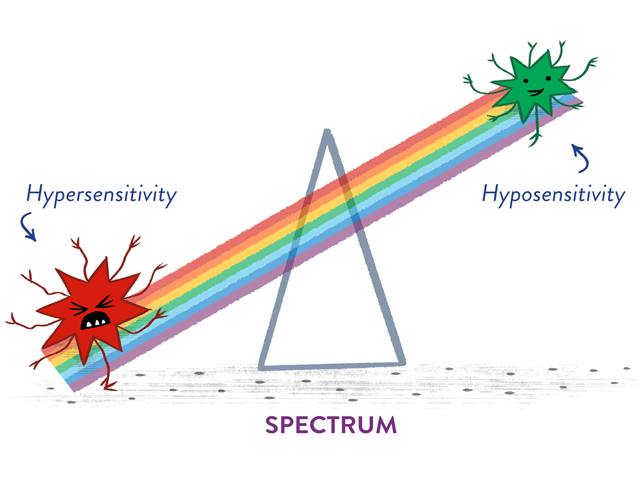
For people with autism, pain perception can be even more unique. Some may experience “hypersensitivity,” where they feel intense pain from what can seem like minor sensory inputs like a cut or loud noise. For some, a light touch might feel unbearable. Other people with autism may go in the opposite direction and have “hyposensitivity.” where they barely feel any pain, even with serious injuries like broken bones.
The way an Autistic person reacts to pain can also be different. Sometimes, they might not show they are in pain the way others do. Instead of crying or saying “owww” they might become quiet, seem frustrated, or seek other sensory input. This can make it hard for others to know when they are hurting
All these factors can create major barriers to getting the right treatment or response from the people around them. It can mean that people with Autism can be in unnecessary pain that could be avoided.
Pain Scales Aren’t Universal
If you’re seeing a medical provider about something that hurts, they might ask you to rate your pain on a scale, like using the Faces scale or ranking your pain from 0-10. Pain scales are designed to standardize how patients report their pain, but that is limited by the very different ways people experience and communicate pain. Typical pain scales often don’t work well for Autistic people because of the generally more atypical way they process information, process sensory input, and communicate.
For example, for Autistic individuals who don’t use speech to communicate, it might be difficult to let someone know their pain level if they don’t have the language tools to match the message they want to express. Also, people with Autism are often very concrete in how they think about the world and their experience. Trying to accurately describe the subjective and rather abstract concept of pain can be a challenge.
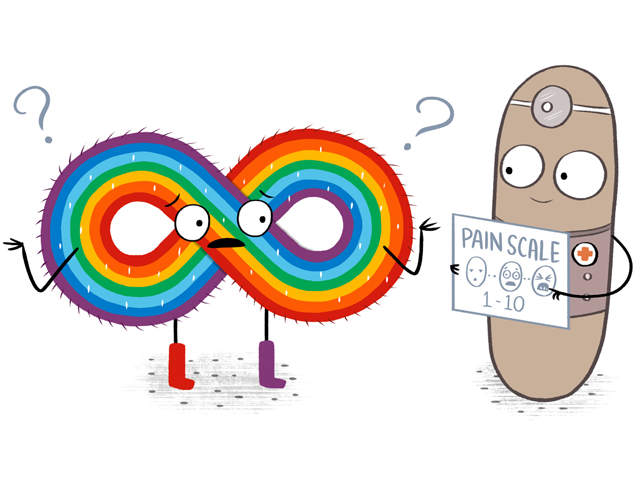
Pain scales rely on abstract concepts like mild, moderate, or severe pain, or cartoon faces that range from smiling to frowning. These types of scales might not make sense for the generally more concrete thinking of Autistic individuals who also may have difficulty accurately interpreting facial expressions.
Communication May Be Different
A large reason pain can be difficult to manage for Autistic people is differences in communication. Some people may not be able to tell you verbally that something hurts. Possible differences in non-verbal communication can mean a person might not show the same body language cues often associated with pain, like wincing or grimacing.
That’s why it’s important for family, friends, and healthcare providers to be extra observant. Family and friends who know the patient well and can better notice differences from usual behavior and understand the various ways the person communicates should be included in healthcare conversations. Changes in behavior, like becoming more quiet, reserved or irritable, can be a way of communicating pain.
How to Help
Let’s talk about the many ways we can help work around these barriers so that people with Autism get the care they need when they are in pain.
Listen:
Most importantly, the voices of Autistic individuals must be heard and respected. Listening to how they describe their experiences with pain, either through speech, AAC (Augmentative and Alternative Communication: using communicative systems that may be alternative to speech), or written communication is critical to providing compassionate and effective care. Taking the time to discover how they communicate best is key.
Be curious:
Pay attention to any changes in behavior, mood or habits. Someone that is exhibiting what is typically considered “challenging behaviors” might actually be communicating their pain. Stay curious to figure out the root cause of a behavior. For healthcare providers, friends and family members can be helpful allies in this process.
Ask in different ways:
If you think someone is in pain but they are not able to tell you directly, try asking in different ways. You could ask something concrete like “Does the hurt make it hard to walk on your ankle?” “Is there a part of your body that is bothering you? or “Does your head hurt?” The more concrete you are, the easier it is to gather useful information. Sometimes showing pictures or using tools like Communication Boards can help them show where it hurts. Remember to be patient. It can take time for Autistic people to express that they are in pain. Give them tools and space to communicate how they feel, in their own way.
Create comfortable spaces:
A higher than usual sensitivity to sensory input is common for people with Autism. Bright lights, loud sounds, or rough textures can overstimulate the nervous system and make pain worse. Taking the time to create a quieter, more comfortable environment can be part of a comprehensive plan to address pain for Autistic individuals. This can start with even small gestures like speaking a quieter, calmer voice.
Train Healthcare Providers:
It starts with awareness. Doctors, nurses, and other professionals need to understand that 1) pain might show up differently for someone with Autism that it would in someone who is neurotypical AND 2) it is NOT going to show up the same way in each Autistic individual. Learning more about Autism can help providers offer quality healthcare to Autistic people. This blog is a good start, but for more information, please visit the Autism Society’s Training and Resource Center.
It Really Does Matter
We all need to recognize that we don’t all have the same experiences. Regardless of whether we understand another person’s experience of pain, everyone deserves to have their pain taken seriously. Bad pain experiences can lead to unnecessary suffering, and have long term consequences like medical trauma and avoiding getting health care in the future.
When we recognize that everyone’s pain experience is unique, we become more empathic, caring and supportive. This helps individuals get the care they need, feel more comfortable, and live healthier lives. Let’s work together to make sure no one’s pain goes unnoticed.
To learn more about the Autism Society of America, please visit AutismSociety.org
To learn more about our successful strategies used in the Autism Society’s Vaccine Education Initiative, please visit AutismSociety.org/vei.
To learn more about training opportunities, please visit the Autism Society’s Training & Resource Center.
You May Also Be Interested In
Blog Post
Getting to know CHYP and their innovative approach to chronic pain
CHYP is an online nonprofit for youth ages 13-24 that was built on the understanding that creative techniques – be it writing, yoga, art, acupuncture or other immersive experiences – can help rewire the nervous system’s pain routes.
Blog Post
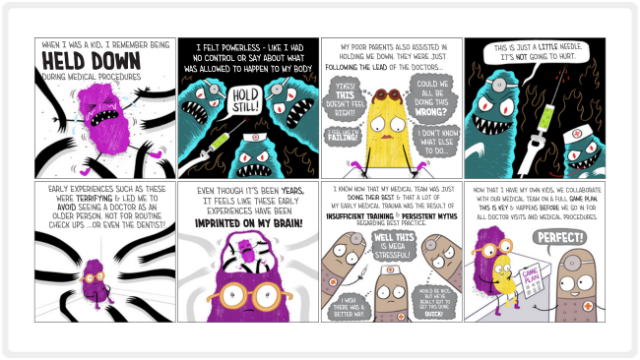
Can holding children down for shots traumatize them? A health psychologist says yes.
I’m a health psychologist and expert in medical illness, trauma, and pain, with 25 years of experience. If I could wipe out any practice that happens on the daily in medicine, VERY high on my list is holding down kids for medical procedures. While science and best practice guidelines from top medical organizations clearly say holding down kids is a terrible idea, it still happens every single day.

Blog Post
Getting to know ChildKind International: Intro to the International Certification Organization for Pediatric Pain
Julia Johnston, a Knowledge Management Specialist at ChildKind International, is your guide to understanding ChildKind's institutional certification process and crafting valuable resources.

Blog Post
How to Make Shots Hurt Less for Kids and Overcome Needle Phobia
Get ready for Needle Poke Game Day with these expert, research-backed strategies for getting your kiddo through a needle poke with more comfort and less pain– Yes, really! These strategies help shots hurt less!

Blog Post
No Shame In This Game: Supporting Tweens and Teens Through Needle Anxiety
Being a teenager is all about independence and having more control of their lives. Needle fears can get in the way of them taking control of their healthcare. Here is what teens and their adults can do that really helps.

About the Author
Danielle Hall is the Director, Health Equity Initiative at the Autism Society. Danielle has a Master’s Degree in Social Work with an emphasis on Public Health. She brings more than 20 years of experience in planning, designing, evaluating, and managing programs to promote health, equity, and access. Danielle lives in New Jersey with her husband, two girls, and Cocker Spaniel.