Nine reasons why pain management is a big deal
Even though we all live with it, we still get asked—usually by someone who isn’t currently in pain—‘Is it really that big a deal?’ As a pain nonprofit, we can say with complete confidence: Heck yes, it is!
Jody Thomas, PhD
Babies & Toddlers (0-2) Kids (3-11) Tweens & Teens (12+) Acute Pain Chronic Pain Procedural Pain
Share this:
If you’ve ever cared for a child in pain, you’ve probably felt it—that gut-wrenching mix of uncertainty, fear, and helplessness, wondering what to do and how to make it stop. As a parent, caregiver, or healthcare professional, we’ve all been there. You also undoubtedly have difficult memories about your own pain experiences as a kid. Maybe it’s hard to consider how much they affect you even today. If so, you’re not alone. Pain is a universal experience that touches us all.
Even though we all live with it, we still get asked—usually by someone who isn’t currently in pain—‘Is it really that big a deal?’
As a pain nonprofit, we can say with complete confidence: Heck yes, it is!

This isn’t just a matter of personal opinion or even professional experience. Decades of research and thousands of studies establish that it is a scientific fact. What’s more, this research shows there are practical, effective solutions that many people simply don’t know about. So, let’s dive into nine reasons why pain management is, without question, a big deal.
1. Every day, kids (and adults) experience pain that is avoidable and unnecessary.
We can all agree that this is ridiculous and unacceptable. The reasons why this happens are complex but here is the bottom line: pain management techniques that are scientifically proven and endorsed by leading medical organizations often fail to make their way into everyday healthcare.
Adding to the problem is the massive gap between what most people know about pain and what they need to know to feel more comfortable and in control. The result? Unnecessary suffering for millions of kids and adults.
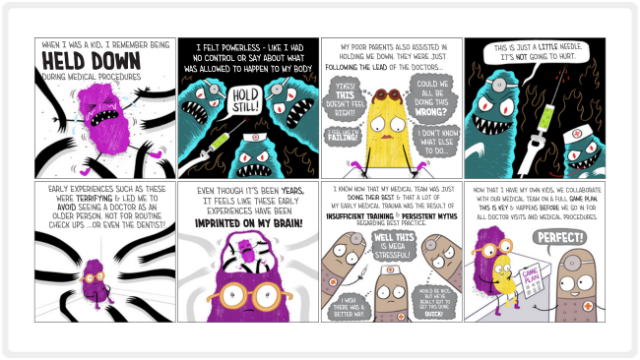
2. Early pain experiences shape how kids experience and cope with pain as adults
Mismanaged pain in childhood is about much more than “just a hard few minutes” at the doctor’s office, or a “a bit of a rough time” after surgery in the hospital. It’s not just about the next five minutes—it’s about the next 50 years. What might seem like temporary discomfort often has permanent effects. It actually rewires the brain and body, even in babies that won’t consciously remember exactly what happened.
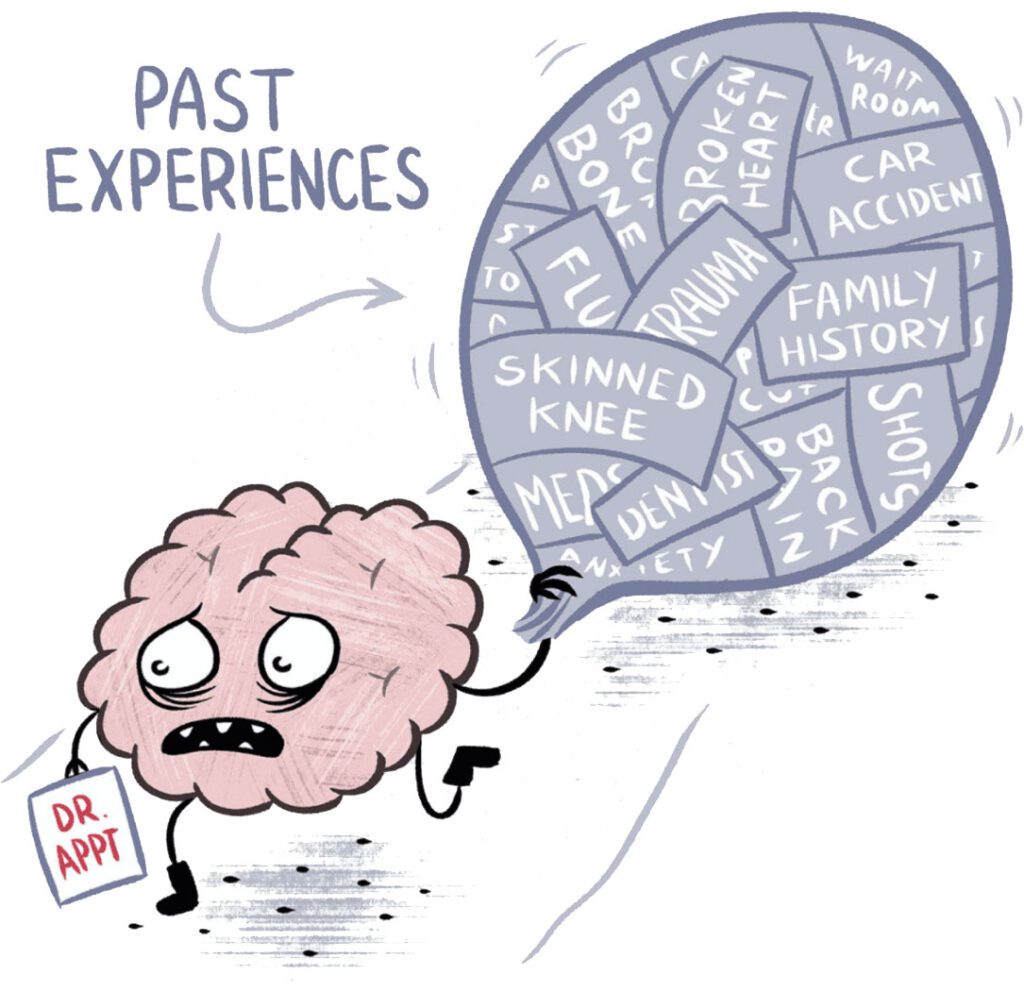
These early experiences can lead to long-term trauma, healthcare avoidance, and preventable health problems. They increase the risk of chronic pain, anxiety, depression, substance abuse, problems sleeping, and so much more. And the psychological scars left by poorly managed pain create ripple effects that impact health, mental well-being, and trust in doctors.
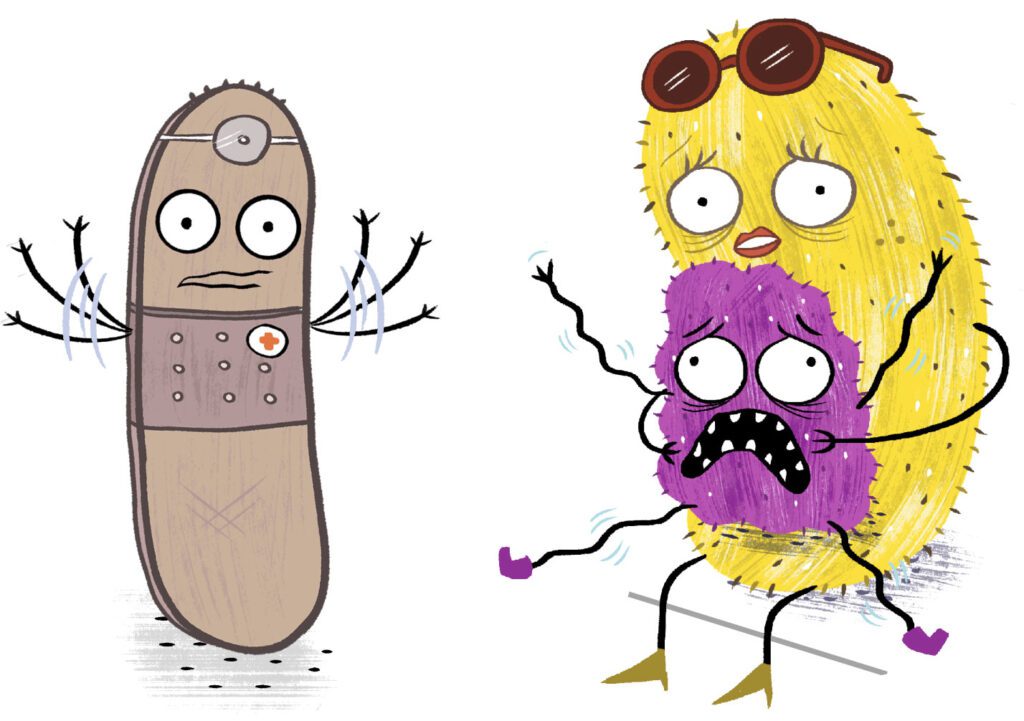
3. Needle anxiety often starts with those first shots.
That badly handled vaccine or blood test where no one bothered to do any pain management? That one where someone ended up being held down and screaming? It is directly related to the 63% of kids, 50% of teens, and 25% of adults who have enough needle anxiety to change their health care decisions. It’s also related to the worried look on your kid’s face when you talk about going to the pediatrician and your teen’s refusal to get that cancer preventing vaccine.
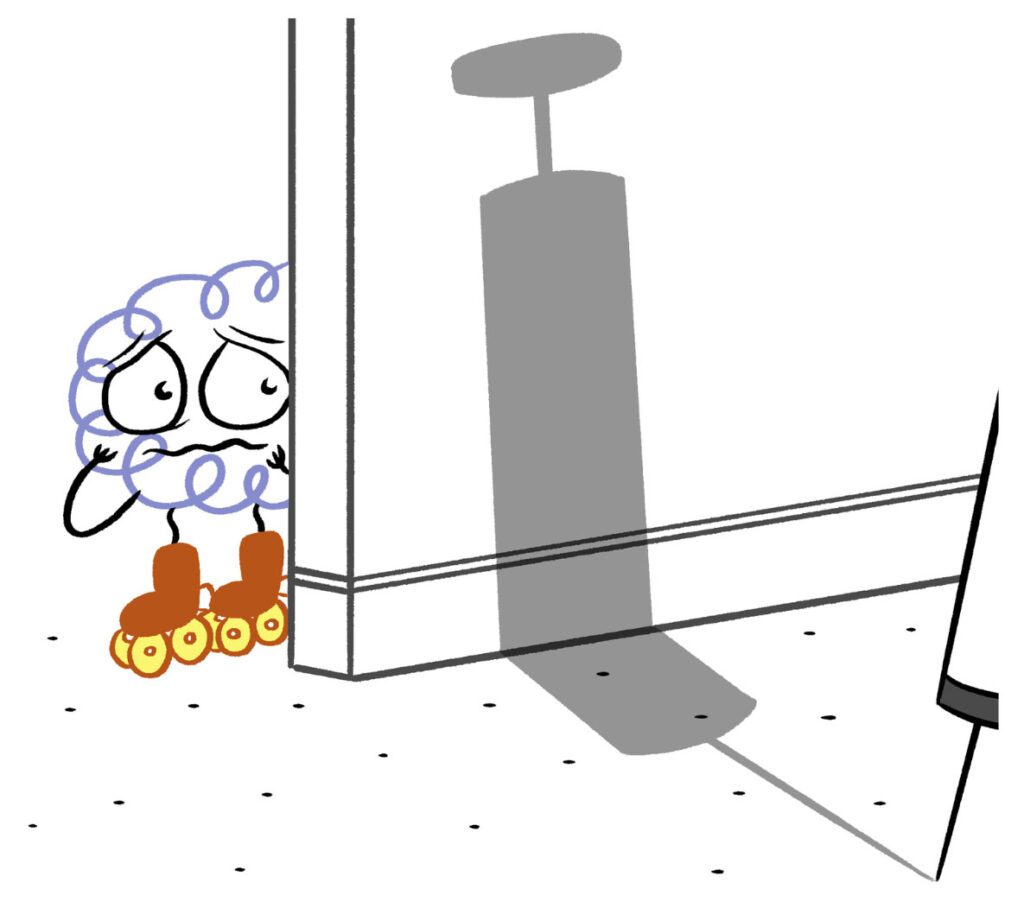
You know that adult friend or family member that you worry about because they won’t go get that concerning symptom checked out and haven’t had a blood test in years? It is extremely likely that avoidance of health care started with a hard needle stick as a small child. This avoidance affects everything—from early disease detection (avoiding those check-up appointments) to getting vaccinated and following medical advice. And the consequences reach far beyond any single person, influencing public health at a very large scale.
4. Simple, effective solutions exist—and work.
If we had a dollar for every time someone was shocked to learn that strategies like numbing cream, vibration, comfort positioning, and distraction can effectively reduce needle pain and anxiety, we could fund the Meg Foundation for years! And we’d also have a lot less adults break down in tears, upset that knowing earlier could have prevented years of suffering. These strategies aren’t just nice-to-haves—they’re backed by science. Yet a shocking number of families and healthcare providers don’t know about them.

At the Meg Foundation we create resources that are free and easy to use because knowing better means doing better. We believe in the power of turning information into life changing action. It’s not just for medical procedures. Effective tools exist for acute pain (think broken bone or knee surgery) and chronic pain (those nagging headaches or ongoing body pain) too. We just need to get them into the right hands, your hands to be exact.
5. Pain is a biological, psychological, and yes, social experience.
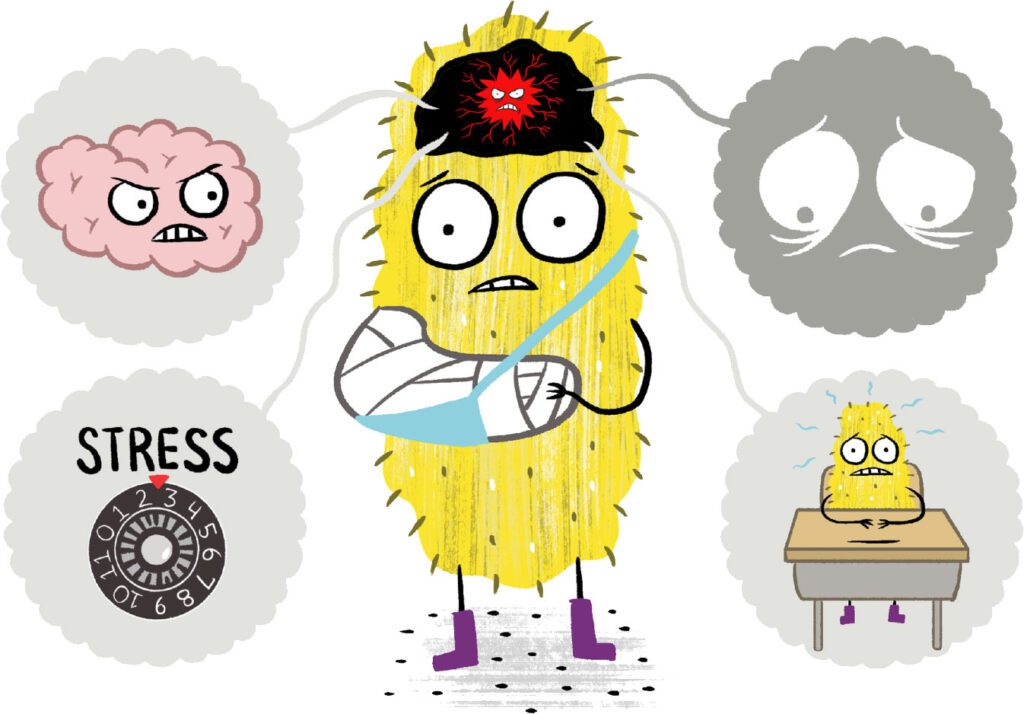
Most people, including some in the medical field, still incorrectly believe that pain is just a straightforward biological experience. Decades of research tells us it’s not that simple. Our psychological state, our mindset, our personal history, our environment, and the people around us all play a major role in the experience of pain.
If you think about it, this also matches up with your own experience. Ever notice how it hurts worse when you stub your toe when you are in a bad mood than when you are in a good mood? Can you think of a time when things got worse because someone didn’t believe you were hurting? What about that blister on your foot that hurt a lot worse after you looked at it? You weren’t being dramatic: those factors actually change the process of pain.
6. The fact that pain is complex is actually GREAT news.
Why? Because it opens up so many more possibilities for finding comfort and control. It means we can go far beyond the limits of things like medications or surgeries to find relief. Meds have an important role in pain management, but anyone who’s ever used them can tell you that they don’t work quick enough, well enough, or long enough. It doesn’t solve the whole problem because it’s just one part of the puzzle.
We all need to understand things like movement can often be medicine, what’s going on in the world around us matters, and psychotherapy can be a game changer in recovery. Embracing this biopsychosocial model of pain (we know, long jargon-y word but stick with us) doesn’t just help you as an individual. It also opens up possibilities of making progress on some of the larger challenges in healthcare.
7. Chronic pain is the leading drain on the U.S. healthcare system.
It costs us billions of dollars a year and is also the leading cause of disability for adults in the US. Where do those patterns start? Childhood. Doing it right from the beginning by equipping families and kids with the tools they need is the way we stop this problem before it starts.
Addressing pain early isn’t just the right thing to do—it’s cost-effective. It saves money, time, and resources while improving peoples’ lives and bettering healthcare in the process. It also brings relief to the 20% of kids that struggle with chronic pain. Seems like a win all the way around, right?
8. It’s a huge burden on health care workers.
Not surprisingly, dealing with patients’ pain is one of the most stressful parts of a healthcare worker’s job. When they can manage pain effectively, everyone benefits—patients, families, and the providers themselves.
Let’s be real, with burnout at an all time high, it has never felt more important than now to champion the people who spend their days taking care of our health and well-being. All of us at the Meg Foundation are dedicated to making it easier for them to provide the highest level of care. The goal is to ease their burden by giving them the tools, resources, and training they need.
9. We can do better – and it’s not that hard.
The solutions are there; we just need to implement them. By harnessing the power of tech, science, and design, we can change lives and ease suffering. It’s about being creative about how we get the right solutions into the hands of people who need them so they can turn information into action. It’s about how we get you what you need, whether you are in the doctor’s office, the ER waiting room, or your own living room.
By closing the gap between research and practice, we can prevent needless pain, empower families, and create a healthier future—for everyone.
What’s the take home message?
Pain during childhood has a lasting impact on mental and physical health. When pain isn’t addressed well, kids carry the effects with them into adulthood, often facing greater health risks, deeper emotional struggles, and a lifelong wariness of healthcare.
The trauma from under-treated pain can ripple through their lives, creating physical and psychological changes, and can lead to poorer health choices down the road. This is why proper pain care isn’t just important—it’s essential for helping kids build healthier futures. Research has shown us better ways, but the gap between what we know and what’s practiced is wide.
We’re here to close the gap—so kids don’t just ‘tough out’ pain but can confidently manage it.
We’re here to make sure no child hurts when they don’t need to.
We’re here to empower all families, including yours.
Now, we need your help to make it all happen. Because yes, pain management is truly a big deal.
You may also be interested in
Blog Post
Chronic Pain Is On The Rise—Here’s What You Can Do About It Now
Earlier this week, The Washington Post featured a startling stat in their Big Number series: nearly 1 in 4 adults in the U.S. experienced chronic pain last year. And that is up from 20.4% in 2019! Let that sink in.
Blog Post
Can holding children down for shots traumatize them? A health psychologist says yes.
I’m a health psychologist and expert in medical illness, trauma, and pain, with 25 years of experience. If I could wipe out any practice that happens on the daily in medicine, VERY high on my list is holding down kids for medical procedures. While science and best practice guidelines from top medical organizations clearly say holding down kids is a terrible idea, it still happens every single day.

About the Author
Dr. Jody Thomas is a licensed clinical psychologist, and specialist in pediatric medical illness and trauma. A well-known expert in pediatric pain who teaches internationally on the subject, she is also a founder and the former Clinical Director of the Packard Pediatric Pain Rehabilitation Center at Stanford, and a former Assistant Professor at the Stanford University School of Medicine. Though she now lives in Denver, CO, she still serves as Adjunct Faculty for Stanford, providing supervision and teaching. As a consultant for the Lucile Packard Children’s Hospital at Stanford, she directs projects on the integration and innovation of pain management using tech-based intervention. Her passion for bringing together the power of medical science, technology and design to transform the way we think about kids and pain led her to her current focus but it’s her role as a mom of two that solidified her path in creating the Meg Foundation.